Aviragen Therapeutics
Aviragen Therapeutics (AVIR) is focused on the discovery and development of direct-acting antivirals to treat infections that have limited therapeutic options and affect a significant number of patients globally. The Company has three Phase 2 clinical stage compounds: BTA074, an antiviral treatment for condyloma caused by human papillomavirus types 6 & 11; vapendavir, a capsid inhibitor for the prevention or treatment of rhinovirus (RV) upper respiratory infections; and BTA585 (enzaplatovir), a fusion protein inhibitor in development for the treatment of respiratory syncytial virus infections. The company also have a preclinical RSV non-fusion inhibitor program.
In April 2017, the company engaged Stifel, Nicolaus and Company, Incorporated (“Stifel”) as its advisor to assist with the exploration of strategic alternatives (the “Strategic Review”). Stifel is providing a range of advisory services aimed to enhance stockholder value. The alternatives to be considered may include, but are not limited to, the potential for a business combination or strategic merger, in-licensing clinical stage programs, an acquisition or other strategic transactions. Aviragen Therapeutics has and expect to continue to devote substantial time and resources to exploring strategic alternatives; however, there can be no assurance that such activities will result in any agreements or transactions that will enhance stockholder value. In addition, potential strategic transactions that require stockholder approval may not be approved by its stockholders. Further, any strategic transaction that is completed ultimately may not deliver the anticipated benefits or enhance stockholder value.
Background
Aviragen Therapeutics has historically focused its research and drug development capabilities on discovering and developing small molecule compounds that can prevent or treat infectious diseases. Infectious diseases are caused by pathogens that are present in the environment, such as viruses and bacteria, which enter the body through various means and overwhelm its natural defenses and cause an infection. The severity of an infectious disease varies depending on the nature of the infectious pathogen, as well as the degree to which the body’s immune system or available therapies can prevent or fight the infection. The market for anti-infective drugs can be divided into three general categories: antiviral, antibacterial and antifungal. Aviragen Therapeutics is currently focused on developing antiviral compounds.
The use of antiviral drugs has led to a significant reduction in the morbidity and mortality associated with infectious diseases. However, for many infectious diseases, current treatment options, to the extent any such treatment options are currently available, are associated with suboptimal treatment outcomes, significant toxicities, tolerability issues or adverse side effects, the emergence of drug resistant pathogens, complex dosing schedules, and inconvenient methods of administration. These sub-optimal characteristics of many existing treatment options often lead to patients prematurely discontinuing treatment or not fully complying with treatment dosing schedules, resulting in a treatment failure. A patient’s failure to comply fully with a recommended dosing schedule can also both accelerate and exacerbate the emergence of drug-resistant strains. In recent years, the increasing prevalence of drug-resistant pathogens has created ongoing treatment challenges with respect to many infectious diseases. The ability of viruses to adapt rapidly to existing or new treatments through genetic mutations allows new strains to develop that may be resistant to currently available drugs.
Pipeline
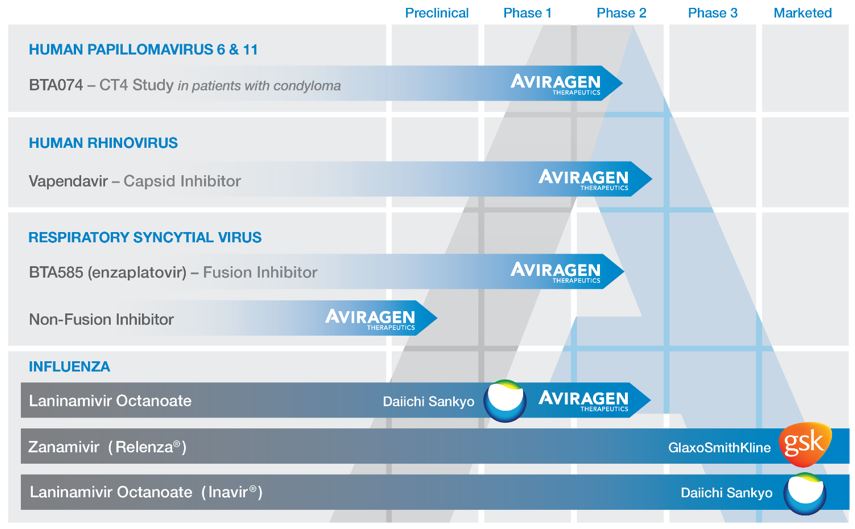
The following chart summarizes key information regarding its antiviral product candidates:
Human Papillomavirus (“HPV”)
HPVs are small non-enveloped, double stranded DNA viruses that infect mucosal or cutaneous squamous epithelia, where they may cause benign or malignant hyperproliferation of the skin and mucosa. HPV is the most common cause of sexually transmitted infection and the disease burden includes skin warts, genital warts, cervical and other anogenital dysplasias and carcinomas, oropharyngeal cancer and recurrent respiratory papillomatosis (“RRP”). Over 40 distinct types of HPV can infect the genital tract. Approximately 90% of infections caused by HPV’s are asymptomatic and resolve spontaneously within two years. However, persistent infection with some HPV types can cause cancer and other benign diseases. Of the 13 HPV types designated as human carcinogens, types 16 and 18 account for 70% of cervical cancers worldwide. Among non-carcinogenic types, HPV 6 and 11 are responsible for 90% of anogenital warts.
Genital warts, also referred to as anogenital warts or condyloma, are the most commonly identified pathology caused by genital HPVs. Genital warts are sexually transmitted, with a high rate of transmission and significant psychosocial morbidity. Genital warts are one of the most common viral sexually transmitted disease (“STD”) worldwide. It is one of the most frequent STDs diagnosed among genitourinary medicine (“GUM”) clinics and accounts for more frequent visits to general practitioners or GUM clinics than those for genital herpes. In 2013, the Centers for Disease Control and Prevention ("CDC") estimated that in the U.S. there were more than 400,000 visits to physicians’ offices related to genital warts.
Currently, no approved HPV-specific direct acting antiviral drugs exist to treat genital warts. Existing t reatments for genital warts can be divided broadly into two categories: provider-administered ablative/cytodestructive therapies (including cryotherapy, laser ablation, and trichloroacetic acid) and patient-administered topical therapies, such as podophyllotoxin, sinecatechins, and imiquimod. Imiquimod directly activates innate immune cells through toll-like receptor 7, resulting in production of cytokines. Treatment choice depends on the morphology, number, and distribution of warts and patient preference. Significant failure and relapse rates, often as much as 20-30% or more have been reported for all of these existing treatments. Further, all existing therapies are associated with local skin reactions including itching, burning, erosions and pain. Therefore, despite the existence of marketed prophylactic vaccines, effective therapies against pathologies caused by HPV6 and HPV11 are still needed.
BTA074
BTA074 is in development for the treatment of genital warts caused by HPV. BTA074 is a potent and selective inhibitor of the interaction between two viral proteins from HPV6 and HPV11, E1 and E2, an interaction that is an essential step for HPV DNA replication and thus, viral production and pathogenesis. This inhibition results from the binding of BTA074 to the E2 protein (Kd=168 nM). BTA074 is a first-in-class directing acting antiviral specific to HPV and possesses new mechanism of action that can be exploited to treat infections caused by HPV types 6 & 11. BTA074 was selected for clinical development among more than 1200 unique compounds tested. BTA074 was developed by combining chemo-informatics modeling and in cellulo screening of E1/E2 protein-protein interactions. These studies showed that BTA074 inhibits the HPV6 and HPV11 E1/E2 interaction or HPV DNA replication in cellulo with an IC50 of 0.5-1 M. The IC 50 represents the concentration of a drug that is required for 50% inhibition of a biological process. Moreover, BTA074 is highly selective for low-risk types HPV 6 and HPV 11, since it does not inhibit replication of HPV 18 or E1/E2 protein interactions of other HPVs.
BTA074 Clinical Trials
Phase 2. The ongoing Phase 2 trial the company initiated in February 2016 is intended to further validate BTA074’s favorable local skin tolerability profile and antiviral activity. The trial is designed as a double-blind placebo controlled, randomized, Phase 2 study the primary objective of which is to assess the safety, tolerability, pharmacokinetics and efficacy of twice daily topical treatments of BTA074 5% gel for up to 16 weeks in approximately 210 genital warts patients. A primary efficacy endpoint is to determine the complete clearance rate for baseline genital warts lesions after twice daily application of BTA074 5% gel or placebo from baseline week 0 visit to the completion of the treatment. The Phase 2 trial is ongoing with completion of enrollment anticipated in the fourth quarter of calendar year 2017. Top-line safety and efficacy data are expected in the second quarter of calendar year 2018.
Phase 2a. In 2013, a Phase 2a clinical trial of BTA074 5% gel was completed. The six-week, Phase 2a study in 24 subjects (16 active; eight placebo) demonstrated that twice daily application of 100 mg BTA074 5% gel had an excellent local skin tolerability profile and resulted in high patient compliance and no patient drop-outs or treatment interruptions. Further, treatment with BTA074 produced a 56% overall response rate and a 38% reduction in mean baseline wart area.
Phase 1b. In 2013, a Phase 1b multicenter, double-blind, randomized, placebo-controlled study in eight genital warts subjects (six active; two placebo) was completed. 100 mg BTA074 5% gel was applied topically twice daily for seven days to the infected area. No adverse events were reported during this study and no clinically relevant findings were observed in clinical examination, laboratory parameters, vital signs or electrocardiogram (“ECG”) parameters.
Human Rhinovirus (“HRV”)
HRV is a non-enveloped, single-stranded virus that belongs to the Picornaviridae family. Currently more than 100 distinct serotypes of HRV are classified into three species, HRV-A, HRV-B, and HRV-C. HRV is the virus that causes the common cold. Primary market research conducted by the IMS Consulting Group on its behalf with pulmonologists, internists and general practitioners indicated that adult asthma and chronic obstructive pulmonary disease (“COPD”) patients experience four to six colds per year. Asthma is a common disease with underlying inflammation of the airways that affects an estimated 300 million people worldwide and 26 million people in the U.S. Respiratory viruses, and in particular HRV, are a significant cause of exacerbations. In a 2014 study of asthma patients with cold-like symptoms, 63% of the patients had respiratory viruses that were detected by qPCR (quantitative polymerase chain reaction) and the majority of those samples (68%) contained HRV.
COPD is the most common chronic respiratory condition in adults whose prevalence is expected to continue to increase in the future. Currently, the World Health Organization (“WHO”) estimates that 64 million people have moderate to severe COPD worldwide. In the U.S. there are an estimated 28 million individuals over the age of 40 with COPD, with an annual average growth rate of 1.9%. Further, of the estimated 28 million COPD patients in the U.S., approximately 13 million are classified as having moderate to severe/very severe COPD.
Similar to the presence of HRV in asthma exacerbations, HRV is the most common virus detected during exacerbations of COPD. In COPD patients, colds often precede exacerbation symptoms. In a published experimental challenge study, COPD patients with an HRV infection showed more severe and prolonged lower respiratory symptoms, airway obstruction, and neutrophilic airway inflammation than subjects without COPD. In addition, a recent natural exposure study in COPD patients demonstrated that HRV prevalence and viral load at exacerbation presentation were significantly higher compared to a period when the patient was not experiencing an exacerbation. Further, the HRV viral load was elevated in COPD patients that presented to the clinic, consistent with the experimental challenge study, suggesting that viral replication may be ongoing, and antiviral therapy may be an effective treatment modality to prevent or reduce the severity of exacerbations.
There are currently no direct antiviral drugs approved for the treatment of HRV. As such, there remains a significant unmet medical need to identify treatments that can reduce the impact that HRV infection has on the frequency of exacerbations and loss of control, prevent viral transmission, lessen the severity and duration of cold-like HRV symptoms and minimize secondary bacterial infections in asthma and COPD patients.
Vapendavir (BTA798)
Aviragen Therapeutics is developing vapendavir (BTA798), a potent antiviral capsid binder that is designed to bind to a highly conserved pocket in the HRV capsid and interfere with receptor binding and/or related early steps in the infectious cycle. Vapendavir is a potent inhibitor of picornaviruses and has been shown to inhibit the replication of a wide range of HRV serotypes and the replication of a majority of recent HRV clinical isolates in tissue culture assays. The median EC50 value for vapendavir against the 100 HRV serotypes is a potent 5.8 ng/mL (15.2 nM). The EC50 represents the concentration of drug that is required for 50% inhibition of viral replication in vitro. Vapendavir has also demonstrated antiviral activity against other clinically relevant enteroviruses (“EV”) including EV-71 and poliovirus types 1, 2 and 3.
Vapendavir (BTA798) Clinical Trials
Phase 2b SPIRITUS Trial. In February 2017, the Company announced top-line data from its Phase 2b SPIRITUS trial, a multi-center, randomized, double-blind, placebo controlled, dose-ranging study of vapendavir in 454 moderate to severe asthmatics with a rhinovirus infection. Vapendavir did not demonstrate a statistically significant reduction in the primary endpoint, asthma control questionnaire-6 (ACQ-6) at day 14 compared to placebo; however, Vapendavir did demonstrate an antiviral effect and clinical benefit in subjects dosed within 24 hours of symptom onset, consistent with that observed in earlier clinical trials with the drug. The Company is working with several key opinion leaders in evaluating a potential clinical development path for the drug based on the consistent antiviral effect observed in all of its Phase 2 clinical studies and its favorable safety profile.
Phase 1 Bioavailability Trial. In 2016, the company initiated a single-center, open-label, three-period comparative bioavailability study in healthy volunteers to assess the comparability of the vapendavir phosphate salt capsule, and two new formulations of vapendavir free base in the forms of an oral suspension and tablet. Forty-six (46) subjects completed three periods of dosing and the plasma pharmacokinetic results indicated that the bioavailability of the oral suspension and tablet formulations were comparable to the capsule form of vapendavir. The oral suspension formulation is intended to enable the conduct of future pediatric trials, and the tablet formulation will allow an increase in manufacturing scale appropriate for Phase 3 trials and commercial development.
Phase 1 Drug-Drug Interaction Trial. In 2014, the company also completed a drug-drug interaction study entitled ‘A Phase 1, Randomized, Open-Label Study to Evaluate the Effect of Vapendavir (BTA798) on the Pharmacokinetics of Orally Administered Midazolam, a CYP3A4 Substrate, in Healthy Male and Female Volunteers’. This study was designed to assess the effect of vapendavir on the PK profile of midazolam, a CYP3A4 substrate. Additionally, the effect of midazolam on the PK profile of vapendavir, the PK profile differences of vapendavir in males and females, and the safety profile of vapendavir were assessed. Twelve (12) male and 12 female subjects aged 18 to 55 years were randomized to receive one of two oral doses of vapendavir and midazolam. Of the 24 subjects randomized, 22 completed all study visits. No serious adverse events (“SAEs”) occurred during the study. The results of the study confirmed vapendavir’s pharmacokinetic profile as established in prior clinical trials and established that vapendavir is a weak to moderate inducer of CYP3A4, which suggests that vapendavir may be used to treat asthma and COPD patients receiving multiple background medications.
Phase 2. In 2012, the company completed a 300-patient, multicenter, randomized, double-blind, placebo-controlled study of vapendavir in adults with mild to moderate asthma that had a symptomatic HRV infection. The primary objective of the study was to determine the efficacy of vapendavir on symptoms of presumptive HRV infection in asthmatic adults, as measured by the WURSS-21 severity scores. Vapendavir was dosed at 264 mg twice daily for six days. The study was conducted over two HRV seasons (18 months) and 155 subjects in the vapendavir arm and 145 subjects in the placebo group were randomized into the study. The trial successfully met its primary endpoint, which was a reduction of cold symptoms based on the WURSS-21 severity score averaged over days two through day four. The mean daily reduction in WURSS-21 severity score averaged over days two to four was significantly greater in the vapendavir treated group compared to the placebo group (least square mean difference: -4.01, p = 0.020). Vapendavir was generally tolerated and most treatment-related adverse events were of mild intensity, with moderate treatment-related events reported in 2.3% of subjects. No SAE’s occurred during the study.
Phase 2 HRV39 Challenge Study. In 2009, the company completed a Phase 2a placebo-controlled, double-blind, randomized, parallel group trial to determine the potential of 16.5 mg, 66 mg and 264 mg of vapendavir, when dosed twice daily for 10 days, to prevent experimental HRV39 infection (challenge design) in 41 healthy volunteers. Subjects that received 264 mg of vapendavir achieved a statistically significant reduction compared to placebo in mean viral load on days two to five inclusive. Vapendavir was generally well tolerated, and the overall incidence of adverse events was low, not dose dependent, and was similar to placebo. There was one SAE of neutropenic sepsis in a subject in the 66 mg arm of the trial.
Respiratory Syncytial Virus (“RSV”)
RSV, a member of the Paramyxoviridae family of viruses, is a major cause of acute upper and lower respiratory tract infections in infants, young children, and adults. Datamonitor, an independent research provider, estimates that approximately 18 million people are infected annually with RSV in the seven major markets worldwide, including over 9 million children under the age of four, 5.5 million elderly, and 3 million adults with underlying disease. About 900,000 of these individuals are hospitalized for their RSV infection. These infections are particularly problematic in infants, as approximately 91,000 are hospitalized with RSV infection in the U.S. in any given year. RSV infections are also responsible for 40% to 50% of hospitalizations for pediatric bronchiolitis and 25% of hospitalizations for pediatric pneumonia. In addition to pediatric patients, elderly patients with cardiac or pulmonary conditions and adults that have received a hematopoietic stem cell transplant are at an increased risk for severe RSV infection. The overall magnitude of hospitalizations makes RSV a costly disease, although mortality is low.
To date, only three drugs have been approved to either prevent or treat RSV infections. Ribavirin is used to treat serious RSV infections in infants with severe bronchiolitis and in immunocompromised patients. However, its use is restricted due to highly variable efficacy and toxicity risks. In fact, current American Academy of Pediatrics guidelines for the treatment of bronchiolitis in children do not recommend the routine use of ribavirin to treat RSV infection due to lack of clinical evidence supporting its use. Antibody-based products RespiGam® (no longer available) and Synagis® (palivizumab) were designed, developed and approved to prevent, not treat, RSV infections in high risk premature infants. Due to the high cost of treatment with Synagis®, its use is limited in many hospitals. There remains a significant unmet need for a safe and effective treatment for RSV in all at-risk populations.
BTA585 (enzaplatovir)
Aviragen Therapeutics's lead compound, BTA585, is a potent, non-cytotoxic and selective inhibitor of the RSV F protein. Data from studies investigating the mechanism of BTA585 antiviral activity, including analysis of RSV resistance mutants, support the conclusion that BTA585 inhibits the function of the RSV F protein. Therefore, BTA585 exerts its antiviral activity by interfering with the earliest stage of infection by inhibiting the attachment and/or fusion of the virus to the host cell. BTA585 is equally active against both RSV A and B subtypes but has no known activity against other pathogenic viruses. When tested in vitro against a panel of RSV A & B clinical isolates, BTA585 was found to be potent with an average EC50 =138nM.
BTA585 Clinical Trials
The double-blind, placebo-controlled, Phase 2a trial initiated in April 2016 in the U.K. was designed to evaluate the safety, pharmacokinetics, and antiviral activity of orally dosed BTA585 in healthy volunteers challenged intranasally with RSV-A Memphis 37b. Following intranasal inoculation with RSV, and a positive test for RSV or five days after challenge, approximately 60 healthy adults were randomized to receive either BTA585 400 mg BID, BTA585 600 mg BID, or placebo, dosed twice daily for seven days and monitored for 28 days.
In February 2017, the Company announced top-line data from its double-blind, placebo-controlled Phase 2a study of BTA585 in adults challenged intranasally with RSV. The data indicated there was not a significant reduction in the primary endpoint, which was change in AUC viral load (copies/mL*hours) from first dose of study drug through study day 12. The overall safety profile of BTA585 was favorable and consistent across treatment groups. Further analysis of the pharmacokinetic/pharmadynamic results from patients in the trial suggested that the systemic concentration of BTA585 was not sustained above the EC90 for the challenge RSV-A strain Memphis 37b over the duration of dosing period potentially contributing to sub-therapeutic antiviral levels.
During the Phase 2a trial, in May 2016, the company announced a voluntary delay in enrollment due to the receipt of a lab result from one subject showing an increase of a cardiac enzyme level coupled with transient ECG changes, which led to a hospitalization of less than 24 hours for observation and assessment. The subject's ECGs normalized in the clinic prior to hospitalization and the cardiac enzyme levels returned to baseline shortly thereafter. Furthermore, a cardiac MRI was normal with no evidence of functional deficit or ongoing cardiac condition. After a review of the subject’s data, the MHRA agreed to allow enrollment to resume in order to complete the higher dose level cohort. The company also reported that subsequent to the submission of the requisite safety report of this event to the FDA, the company received communication from the FDA that the investigational new drug application (“IND”) for BTA585 had been placed on clinical hold for future studies being conducted in the U.S. under the IND. In the first half of calendar 2017, the Company had completed the requested non-clinical studies requested by the FDA to support a response to the clinical hold, but has subsequently put all activities related to the BTA585 program on hold until completion of the Company’s Strategic Review process.
Phase 1 Multiple Ascending Dose (“MAD”) Clinical Trial
In 2016, the company completed a blinded, placebo-controlled MAD study, conducted in the U.S. under an IND, which evaluated the safety and PK of three cohorts of healthy volunteers (100, 400, and 600 mg BTA585) dosed orally twice a day for seven consecutive days. Each of the dose cohorts consisted of eight subjects that received BTA585 and four that received placebo. Adverse events occurring in more than two BTA585-treated subjects were headache and chromaturia. Additional results showed that BTA585 plasma Cmax was rapidly achieved at approximately one hour following oral dosing, exposure was dose-proportional, there was no accumulation of BTA585 over the duration of dosing and the half-life (T1/2) was approximately 5 to 6 hours.
Phase 1 Single Ascending Dose (“SAD”) Clinical Trial
In 2016, the company completed a blinded, placebo-controlled SAD study, which was conducted in the U.S. under an IND, evaluating the safety and pharmacokinetics (“PK”) of six oral doses of BTA585 (50, 100, 200, 400, 500 and 800 mg) in healthy volunteers. In addition, the 100 mg cohort included an evaluation of the effect of food on the PK profile of BTA585. Each of the dose cohorts consisted of seven subjects that received BTA585 and three that received placebo. Overall, there was low incidence of adverse events (“AEs”) with BTA585 treatment. AEs occurring in more than two BTA585-treated subjects included headache, nausea, and chromaturia. In the fasted subjects, pharmacokinetic data demonstrated that doses ≥ 100 mg achieved BTA585 plasma levels that exceeded the mean EC50 of RSV clinical isolates for 24 hours. The BTA585 plasma Cmax was rapidly achieved at approximately one hour following oral dosing and the half-life (T1/2) was approximately 5 to 6 hours. Additionally, dosing of BTA585 with a high fat meal did not adversely affect the PK.
Non-Fusion RSV Inhibitors
In July 2016, the company entered into an exclusive, worldwide license and sponsored research agreement with Georgia State University Research Foundation (“GSURF”) to jointly develop and commercialize RSV replication inhibitors discovered by Professor Richard Plemper and his team in the Institute for Biomedical Sciences (“IBMS”) at Georgia State University. The company believe that RSV replication inhibitors could be useful as a stand-alone treatment or potentially in combination therapy with BTA585 or other RSV therapies for the treatment of patients infected with RSV. Aviragen Therapeutics has commenced research activities using medicinal chemistry to synthesize and potentially identify compounds that have biological activity in screening models of RSV replication inhibition.
Laninamivir Octanoate (“LANI”)
In 2003, the company cross-licensed intellectual property related to a new class of inhaled long acting neuraminidase inhibitors (“NI’s”) with Daiichi Sankyo. The lead product from this collaboration is LANI, also known as CS-8958, a second-generation octanoyl ester pro-drug of laninamivir. LANI has been shown to have in vitro neuraminidase-inhibitory activity against various influenza A and B viruses, including subtypes N1 to N9 and oseltamivir-resistant viruses, and it has also been found to be effective against a swine origin H1N1 strain. Moreover, LANI has long-lasting antiviral activity. LANI was successfully developed by Daiichi Sankyo in Japan and since 2010 has been marketed there as Inavir® for the treatment of influenza A and B infections. In December 2013, Inavir® was approved for use in the post-exposure prevention of influenza.
Strategy
Aviragen Therapeutics is focused on the discovery and development of direct-acting antivirals to treat infections that have limited therapeutic options and affect a significant number of patients globally. In the near-term the company intend to employ the following strategy:
- Focus its resources on the clinical development of its topical antiviral product BTA074 for the treatment of genital warts caused by HPV types 6 & 11 as well as continue preclinical activities related to the RSV non-fusion program. More specifically, over the next 12 months the company intend to:
- File an investigational new drug application to the FDA for BTA074;
- Complete enrollment in Phase 2 BTA074 CT4 study and report top-line data from the trial; and
- Continue research activities to identify a potent, bioavailable, non-fusion RSV clinical candidate.
Research and Development
Aviragen Therapeutics's research and development expense in fiscal 2017 and 2016 was $28.3 million and $26.3 million, respectively. In fiscal 2018, the company plan to focus its research and development resources primarily on ![]() the clinical development of BTA074, and (ii) conduct screening, lead-optimization, and preclinical studies on several series of RSV non-fusion inhibitors.
the clinical development of BTA074, and (ii) conduct screening, lead-optimization, and preclinical studies on several series of RSV non-fusion inhibitors.
The company use third party research firms and consultants extensively to conduct medicinal chemistry, virology, and cell culture assays activities under its management. The company do not have any future plans to build laboratory facilities or hire significant staff to conduct research, discovery and certain development activities.
Sales and Marketing
The company currently do not have any commercialization or sales and marketing capabilities, and Aviragen Therapeutics has no near term plans to invest in or build such capabilities internally. At the appropriate time, the company plan to investigate partnering, collaborating with or licensing certain rights to its development programs to other larger pharmaceutical or biopharmaceutical companies to support the late stage development and commercialization of its product candidates. The company will then evaluate whether partnering with a third party for these activities will be more beneficial than developing the capabilities internally for each of its product candidates.
Manufacturing
The company currently do not own or operate any facilities in which the company can formulate, manufacture, fill or package its product candidates. The company rely on a group of contract manufacturers to produce its drug substance and to fill and package the materials required to conduct clinical trials under current good manufacturing practices, (“cGMP”). Currently, Aviragen Therapeutics has no plans to own or operate such facilities. If an existing contract manufacturer fails to deliver on schedule, or at all, or fails to manufacture its material in accordance with their or its specifications and/or FDA regulations, it could significantly delay or interrupt the development or commercialization of its product candidates and affect its operating results and estimated development timelines. Aviragen Therapeutics has used contract manufacturers to produce all of the clinical trial material used in the preclinical studies and clinical trials Aviragen Therapeutics has conducted to-date.
Competition
The pharmaceutical and biotechnology industries are intensely competitive. Many companies, including biotechnology, chemical and pharmaceutical companies, are actively engaged in activities similar to its, including research and the development of product candidates for the treatment of infectious diseases. Many of these companies have substantially greater financial and other resources, larger research and development staffs, and more extensive marketing and manufacturing capabilities than the company do. In addition, some of them have considerably more experience in preclinical testing, conducting clinical trials and other regulatory approval procedures. There are also academic institutions, governmental agencies and other research organizations that are conducting research in areas of infectious disease which Aviragen Therapeutics is working. The company expect to encounter significant direct competition for any of the product candidates the company plan to develop. Companies that complete clinical trials obtain required regulatory approvals and commence commercial sales of their products before their competitors may achieve a significant competitive advantage.
Currently, there no approved HPV-specific direct acting anti-viral drugs to treat genital warts. Treatments for genital warts can be divided broadly into two categories: provider-administered ablative/cytodestructive therapies (including cryotherapy, laser ablation, and trichloroacetic acid) and patient-administered topical therapies such as podophyllotoxin (Condylox®; Actavis), sinecatechins (Veregen®; Fougera Pharmaceuticals, Inc.), and imiquimod (Zyclara®, Aldara®; Valeant). Aviragen Therapeutics is aware that there are compounds under clinical development to treat genital warts, including Novan’s SB206 and Cassiopea’s CB-06-02. The company anticipate that BTA074, if successfully developed, would directly compete with the patient-applied topical treatments for genital warts. The company believe key differentiating features of BTA074 could be its mechanism of action, favorable local skin tolerability, efficacy, and lower reoccurrence rate. Three prophylactic vaccines, primarily designed to prevent cervical, vulvar, vaginal, and anal cancers, are currently marketed: a bivalent HPV16/18 vaccine (Cervarix®; GSK), quadrivalent HPV16/18/6/11 (Gardasil®; Merck) and the 9-valent HPV 6/11/16/18/33/52/58 (Gardasil®9; Merck). Gardasil® 9 is indicated for females aged 9 through 26 and males aged 9 through 15, to prevent various HPV related cancers and genital warts in both sexes. Gardasil®, Gardasil® 9, and Cervarix® are not known to exhibit a therapeutic effect on existing HPV lesions.
Currently, there are no approved direct-acting antiviral drugs to treat HRV infections. However, its vapendavir product candidate, if successfully developed, would indirectly compete with drugs approved to reduce the incidence of exacerbations or improve lung function in patients with asthma and COPD, such as fluticasone propionate (Advair®), tiotoprium bromide (Spiriva®), fluticasone furoate/vilanterol (Breo Ellipta®), and roflumilast (Daliresp®). In addition to these approved drugs, there are compounds in the clinical development stage that if successfully developed for the treatment of HRV infections could compete with vapendavir.
Effective treatments of RSV infections in pediatrics, the elderly, and the immunocompromised are very limited. Currently, only Virazole® (ribavirin) is indicated for the treatment of hospitalized infants and young children with severe lower respiratory tract infections due to RSV. Aviragen Therapeutics is aware that there are compounds are under development to treat RSV infections, including Gilead’s presatovir, Johnson & Johnson’s JJ-53718678 (ALS-8176), Ablynx’s ALX-0171 and Ark Biosciences’ AK0529. The only approved drug for the prevention of RSV infections in high risk infants is MedImmune’s palivizumab (Synagis®), a monoclonal antibody. There are several vaccines and antibody products designed to prevent RSV infections in clinical development. Among the clinical stage product candidates in development are Novavax’s RSV F vaccine, GSK’s GSK3003898A vaccine, GSK’s GSK3389245A vaccine, Bavarian Nordic’s BN® RSV vaccine, MedImmune’s MEDI ÄM2-2 vaccine and MedImmune’s monoclonal antibody MEDI8897.
Intellectual Property Rights and Patents
Patents and other proprietary intellectual rights are crucial in its business and industry, and establishing and maintaining these rights are essential to justify the cost to develop and commercialize any of its product candidates and products. Aviragen Therapeutics has sought, and intend to continue to seek, viable and strategic intellectual property rights, including, but not limited to, patent protection for its inventions, and intend to rely upon patents, trade secrets, confidential information, know-how, trademarks, improvements in its technological innovations and licensing opportunities to develop and maintain a competitive advantage for its products and product candidates. In order to protect its intellectual property rights, the company typically require employees, consultants, collaborators, advisors, potential partners, service providers and contractors to enter into confidentiality agreements with us, generally stating that they will not disclose its confidential information to third parties for a certain period of time, and will otherwise not use its confidential information for anyone’s benefit but its.
The patent positions of biotechnology and pharmaceutical companies are highly uncertain and involve complex legal and factual questions. Therefore, the patentability of subject matter the company claim in its patent applications, the breadth of the claims ultimately granted, or their enforceability cannot be predicted. For this reason, the company may not have or be able to obtain or maintain worldwide patent protection for any or all of its products and product candidates, and its intellectual property rights may not be protected or legally enforceable in all countries throughout the world. In some cases the company may rely upon data exclusivity or similar exclusivities, although there is no guarantee that such exclusivity will be available or obtained in any jurisdiction. Further, as the publication of discoveries in the scientific and/or patent literature often lags behind the actual discoveries, the company cannot be certain that the company or its licensors were the first to make the inventions described in its patent applications or that the company or its licensors were the first to file patent applications for such inventions.
Pursuant to the terms of the Uruguay Round Agreements Act, patents filed on or after June 8, 1995 in the U. S. have a term of 20 years from the date of filing, regardless of the period of time it may take for the patent to ultimately issue. This may shorten the period of patent protection afforded to its products as patent applications in the biopharmaceutical sector often take considerable time to issue. Under the Drug Price Competition and Patent Term Restoration Act of 1984, a sponsor may obtain marketing exclusivity for a period of time following FDA approval of certain drug applications, regardless of patent status, if the drug is a new chemical entity or if new clinical studies were used to support the marketing application for the drug.
Zanamivir, a neuraminidase inhibitor (“NI”) approved for the treatment and prevention of influenza A and B, is marketed worldwide as Relenza® by GSK. Most of its Relenza® patents have expired and the only substantial remaining intellectual property related to the Relenza® patent portfolio, which is solely owned by it and exclusively licensed to GSK, is scheduled to expire in July 2019 in Japan. On October 18, 2016, the United States Court of Appeals for the Federal Circuit affirmed the rejection of all pending claims of U.S. Patent Application No. 08/737,141. Accordingly, no future United States royalties will be owed by GSK.
LANI, a long acting NI for the treatment and prevention of influenza A and B, is currently marketed as Inavir® in Japan by Daiichi-Sankyo. The patent relating to the structure of LANI expires in 2017 in the U.S., the EU and Japan, although the product has received patent term extension in Japan until 2021 for treatment and 2022 for prevention. The patent relating to hydrates and the crystalline form of LANI actually used in the product expires in 2021 (not including extensions) in the U.S. and EU and in 2024 in Japan. In February 2015, a patent containing claims relevant to the manufacture of Inavir® was issued in Japan and expires in December 2029. The dry-powder inhaler device patent portfolio, which includes TwinCaps®, is owned by Hovione International Limited (“Hovione”) and is exclusively licensed to it and Daiichi Sankyo worldwide for the prevention and treatment of influenza and other influenza-like viral infections. These patents will expire in 2029 in the U.S., and in 2027 in the EU and Japan.
BTA074 is a direct-acting antiviral Aviragen Therapeutics is developing as a treatment for genital warts caused by HPV 6 and 11. The patent containing composition of matter claims expires in the U.S. in 2029, without extensions. A U.S. patent with claims to method of use has been issued and will expire in 2033, without extensions.
Vapendavir is an oral antiviral picornavirus capsid binder Aviragen Therapeutics is currently developing to treat HRV infections. The company exclusively own the vapendavir patent portfolio, and issued claims under this portfolio will begin to expire in some countries in December 2021, not including extensions. Claims from patents related to a compound comprising an anhydrous crystalline free base form of vapendavir and the preferred commercialization form of vapendavir have been allowed in the United States and other countries and extend intellectual property to 2034, without extensions.
The company also own a patent portfolio focused on developing several series of oral antivirals for RSV. Issued patent claims covering the composition of matter for BTA585 will begin to expire in 2031, without extensions.
Patent Term Restoration/Extension and Marketing Exclusivity
Depending upon the timing, duration and specifics of FDA approval for the intended use of its product candidates, some of its U.S. patents may be eligible for limited patent term extension under the Drug Price Competition and Patent Term Restoration Act of 1984, commonly referred to as the Hatch-Waxman Act. The Hatch-Waxman Act permits a patent restoration term, or extension, of up to five years as compensation for patent term lost during product development and the FDA regulatory review process. However, patent term restoration cannot extend the remaining term of a patent beyond a total of 14 years from the product’s approval date. Subject to certain limitations, the patent term restoration period is generally one-half the time between the effective date of an IND and the submission date of a new drug application (“NDA”) plus the time between the submission date of an NDA and the approval of that application, up to a total of five years. Only one patent applicable to an approved drug is eligible for the extension. The application for such extension must be submitted prior to the expiration of the patent and within 60 days of the drug’s approval. The United States Patent and Trademark Office (“USPTO”), in consultation with the FDA, reviews and approves the application for any patent term extension or restoration. Similar provisions are available in Europe and other foreign jurisdictions to extend the term of a patent that covers an approved drug. In the future, the company may apply for restoration of patent term for one or more of its currently owned or licensed patents to add patent life beyond its current expiration date, depending on the expected length of the clinical trials and other factors involved in the filing of the relevant NDA.
Market exclusivity provisions under the Federal Drug, Food and Cosmetic Act (“FDCA”) can also delay the submission or the approval of certain applications of other companies seeking to reference another company’s NDA. The FDCA provides a five-year period of non-patent data exclusivity within the U.S. to the first applicant to obtain approval of an NDA for a new chemical entity. A drug is a new chemical entity if the FDA has not previously approved any other new drug containing the same active moiety, which is the molecule responsible for the action of the drug substance. During the exclusivity period, the FDA may not accept for review an Abbreviated New Drug Application (“ANDA”), or a 505(b)(2) NDA submitted by another company for another version of such drug where the applicant does not own or have a legal right of reference to all the data required for approval. However, an application may be submitted after four years if it contains a certification of patent invalidity or non-infringement to one of the patents listed with the FDA by the innovator NDA holder. The FDCA also provides three years of marketing exclusivity for an NDA, 505(b)(2) NDA or supplement to an existing NDA if new clinical investigations, other than bioavailability studies, that were conducted or sponsored by the applicant are deemed by the FDA to be essential to the approval of the application, for example new indications, dosages or strengths of an existing drug. This three-year exclusivity covers only the conditions associated with the new clinical investigations and does not prohibit the FDA from approving ANDAs for drugs containing the original active agent. Five-year and three-year exclusivity will not delay the submission or approval of a full NDA. However, an applicant submitting a full NDA would be required to conduct or obtain a right of reference to all of the pre-clinical studies and adequate and well-controlled clinical trials necessary to demonstrate safety and effectiveness. The company cannot assure you that the company will be able to take advantage of either the patent term extension or marketing exclusivity provisions of this law.
Pediatric exclusivity is another type of exclusivity available in the U.S. Pediatric exclusivity, if granted, provides an additional six months to existing exclusivity periods and patent terms. This six-month exclusivity, which runs from the end of other exclusivity protection or the patent term, may be granted based on the voluntary completion of a pediatric study in accordance with a FDA request for such a study. The current pediatric exclusivity provision was reauthorized in September 2007 as part of the Food and Drug Administration Amendments Act.
Licenses and Agreements
GSK
In 1990, the company entered into a royalty-bearing research and license agreement with GSK for the development and commercialization of zanamivir, a NI marketed by GSK as Relenza® to prevent and treat influenza. Under the terms of the agreement, the company licensed zanamivir to GSK on an exclusive, worldwide basis and are entitled to receive royalty payments of 7% of GSK's annual net sales of Relenza® in the U.S., Europe, Japan and certain other countries and 10% in Australia, New Zealand, South Africa and Indonesia to the extent that the underlying patents in those respective countries do not expire. Most of its Relenza® issued patents have expired, and the only substantial remaining intellectual property related to the Relenza® patent portfolio is scheduled to expire in July 2019 in Japan.
Daiichi Sankyo
In 2003, the company entered into collaboration and license agreement with Daiichi Sankyo related to the development of second generation long acting NIs, including LANI. Under the collaboration and license agreement, the company and Daiichi Sankyo cross-licensed the right to develop, make, use, sell or offer for sale, or import products based on its respective intellectual property related to its long acting NIs. In the event that the related intellectual property was out-licensed to a third party, the company would share equally with Daiichi Sankyo in any future royalties, license fees, milestones or other payments received from such a licensee. To date, there have been no third-party licenses granted pursuant to this agreement; therefore, a royalty rate on net sales outside of Japan has not been established.
In March 2009, the company entered into a commercialization agreement with Daiichi Sankyo, pursuant to which Daiichi Sankyo obtained exclusive marketing rights in Japan for long acting NIs, including LANI, covered by the 2003 collaboration and license agreement between the parties. In consideration for these rights, Daiichi Sankyo agreed to pay it a royalty rate equal to 4% on net sales in Japan. In September 2010, LANI (Inavir®) was approved for sale by the Japanese Ministry of Health and Welfare for the treatment of influenza in adults and children.
In April 2016, the company entered into a definitive agreement and received a cash payment of $20 million from HealthCare Royalty Partners III, L.P. (“HCRP”) in exchange for a portion of its royalty rights related to Inavir®.
Regulatory Matters
Overview
The preclinical and clinical testing, manufacture, labeling, storage, distribution, promotion, sale, export, reporting and record-keeping of drug products and product candidates is subject to extensive regulation by numerous governmental authorities in the U.S., principally the FDA and corresponding state agencies, and similar regulatory authorities in other countries.
Non-compliance with applicable regulatory requirements can result in, among other things, total or partial suspension of the clinical development, manufacturing and marketing of a product or product candidate, the refusal of the FDA or similar regulatory authorities in other countries to grant marketing approval, the withdrawal of marketing approvals, fines, injunctions, seizure of products and criminal prosecution.
U.S. Regulatory Approval
Pursuant to FDA regulations, Aviragen Therapeutics is required to successfully undertake a long and rigorous development process before any of its product candidates can be approved and marketed or sold in the U.S. This regulatory process typically includes the following steps:
the successful completion of satisfactory preclinical studies under the FDA’s good laboratory practices (“GLP”) regulations; the submission and acceptance of an IND that must be reviewed and accepted by the FDA and become effective before human clinical trials may begin; the approval of an Institutional Review Board (“IRB”) at each site or location where the company plan to conduct a clinical trial to protect the welfare and rights of human subjects in clinical trials; the successful completion of a series of adequate and well-controlled human clinical trials to establish the safety, potency, efficacy and purity of any product candidate for its intended use, which conform to the FDA’s good clinical practice (“GCP”) regulations; the development and demonstration of manufacturing processes that conform to FDA-mandated cGMPs; and the submission to, and review and approval by, the FDA of a NDA prior to any commercial sale or shipment of a product.
Successfully completing this development process requires a substantial amount of time, risk and financial resources. The company cannot assure you that this process will be completed for any of its product candidates, or will result in the granting of an approval for any of its product candidates on a timely basis, if at all, or that the company will have sufficient financial resources to see the process for any of its product candidates through to completion.
Preclinical Studies
Preclinical studies generally include laboratory, or in vitro, evaluation of a product candidate, its chemistry, formulation, stability and toxicity, as well as certain in vivo animal studies to assess its potential safety and biologic activity. The company must submit the results of these preclinical studies, together with other information, including manufacturing records, analytical data and proposed clinical trial protocols, to the FDA as part of an IND, which must be reviewed by the FDA and become effective before the company may begin any human clinical trials. An IND generally becomes effective approximately 30 days after receipt by the FDA, unless the FDA, within this 30-day time period, raises material concerns or questions about the intended conduct of the proposed trials and imposes what is referred to as a clinical hold or partial clinical hold. If one or more of its product candidates is placed on clinical hold, the company may be required to resolve any outstanding issues to the satisfaction of the FDA before the company can begin, or continue, clinical trials of such product candidates.
Certain preclinical studies must be conducted in compliance with the FDA’s GLP regulations and the U.S. Department of Agriculture’s Animal Welfare Act. Violations of these regulations can, in some cases, lead to invalidation of the studies, requiring such studies to be conducted again. Preclinical studies supportive of an IND generally take a year or more to complete, and there is no guarantee that an IND based on those studies will become effective, thus allowing human clinical testing to begin.
Clinical Trials
The clinical trial phase of drug development occurs after a successful IND submission, and involves the activities necessary to demonstrate the safety, tolerability, biologic activity, efficacy and dosage of an investigational new drug substance in humans, as well as the ability to produce the drug substance in accordance with the FDA’s cGMP requirements. Clinical trials are conducted under protocols detailing, among other things, the objectives of the trial and the parameters to be used in assessing the safety and the activity or efficacy of the product candidate. Each clinical trial protocol must be submitted to the FDA under the IND prior to beginning the trial. Each trial, and the related clinical protocol, must be reviewed, approved and conducted under the auspices of an IRB and, with limited exceptions, requires the patient’s informed consent to participate in the trial. Sponsors, investigators, and IRBs also must satisfy extensive GCPs, including regulations and guidelines for obtaining informed consent from the study subjects, complying with the protocol and investigational plan, adequately monitoring the clinical trial, and reporting any SAEs on a timely basis.
Clinical trials to support a NDA for marketing approval are typically conducted in three sequential phases: Phase 1, 2 and 3. Data from these activities are compiled in a NDA for submission to the FDA requesting approval to market the drug. These phases may be compressed, may overlap, or may be omitted in some circumstances. The FDA may also require sponsors to conduct Phase 4 clinical trials after market approval to study certain safety issues or other patient populations.
- Phase 1: After an IND becomes effective, Phase 1 human clinical trials can begin. A product candidate is typically introduced either into healthy human subjects or in certain cases, patients with the medical condition for which the product candidate is intended to be used. Generally, the purpose of a Phase 1 trial is to assess a product candidate’s safety and the ability of the human body to tolerate it at different dose levels. Absorption, metabolism, distribution and pharmacokinetic trials are also generally performed at this stage. Phase 1 trials typically evaluate these aspects of the investigational drug in both single and multiple doses.
- Phase 2: During Phase 2 clinical trials, a product candidate is generally studied in an exploratory trial or trials in a limited number of patients with the disease or medical condition for which it is intended to be used in order to
 further identify any possible adverse side effects and safety risks, (ii) assess the preliminary or potential effectiveness or biologic activity of the product candidate for specific targeted diseases or medical conditions, and (iii) assess dose tolerance and determine the optimal dose for a subsequent Phase 2 or Phase 3 trial. Phase 2 trials generally involve patients who are divided into one or more groups that will get one of several dose levels of the product candidate, and a control group that is not treated with the product candidate but either receives a placebo or a drug already on the market for the same indication. Typically, two or more Phase 2 studies will be conducted for a product candidate prior to advancing to Phase 3.
further identify any possible adverse side effects and safety risks, (ii) assess the preliminary or potential effectiveness or biologic activity of the product candidate for specific targeted diseases or medical conditions, and (iii) assess dose tolerance and determine the optimal dose for a subsequent Phase 2 or Phase 3 trial. Phase 2 trials generally involve patients who are divided into one or more groups that will get one of several dose levels of the product candidate, and a control group that is not treated with the product candidate but either receives a placebo or a drug already on the market for the same indication. Typically, two or more Phase 2 studies will be conducted for a product candidate prior to advancing to Phase 3. - Phase 3: If and when one or more Phase 2 trials demonstrate that a specific dose or range of doses of a product candidate is potentially effective and has an acceptable safety and tolerability profile, one or more Phase 3 trials may be undertaken to further demonstrate or confirm the clinical efficacy and safety of the investigational drug in an expanded patient population, with the goal of evaluating its overall risk-benefit relationship. Phase 3 trials are generally designed to reach a specific goal or end point, the achievement of which is intended to demonstrate the product candidate’s clinical efficacy. The successful demonstration of clinical efficacy and safety in one or more Phase 3 trials is typically a prerequisite to the filing of a NDA for a product candidate.
The sponsor of a clinical-stage development program may request an “end-of-Phase 2 Meeting” with the FDA to assess the safety of the dose regimen to be studied in a Phase 3 clinical trial, to evaluate the planned design of a Phase 3 trial, and to identify any additional information that will be needed to support an NDA. If a Phase 3 clinical trial has been the subject of discussion at an end-of-Phase 2 Meeting, the sponsor may be eligible for a Special Protocol Assessment (“SPA”), a process by which the FDA, at the request of the sponsor, will evaluate the trial protocol and issues relating to the protocol to assess whether it is deemed to be adequate to meet the scientific and regulatory requirements identified by the sponsor. If the FDA and the sponsor reach agreement on the design and size of a Phase 3 clinical trial intended to form the primary basis of an efficacy claim in an NDA, the FDA may reduce the understanding to writing. The SPA, however, is not a guarantee of product approval by the FDA, or approval of any permissible claims about the product.
Throughout the various phases of clinical development, samples of the product candidate made in different batches are tested for stability to establish any shelf life constraints. In addition, large-scale production protocols and written standard operating procedures for each aspect of commercial manufacture and testing must be developed and validated.
Phase 1, 2, and 3 testing may not be completed successfully within any specified time period, if at all. The FDA closely monitors the progress of each of the three phases of clinical development and may, at its discretion, reevaluate, alter, suspend, or terminate further evaluation or trials based upon the data accumulated to that point and the FDA’s assessment of the risk/benefit ratio to the patient. The FDA, the sponsor, a data safety monitoring board or an IRB may suspend or terminate a clinical trial at any time for various reasons, including a finding that the subjects or patients are being exposed to an unacceptable health or safety risk. The FDA can also request additional clinical trials be conducted as a condition to product approval or advancement to the next stage of development. Additionally, new government requirements may be established that could delay or prevent regulatory approval of product candidates under development.
Clinical trials performed outside the U.S. under an IND must meet the same requirements that apply to studies conducted in the U.S. The FDA may also accept a foreign clinical study not conducted under an IND if the study is well-designed, well-conducted, performed by qualified investigators, and conforms to the ethical principles contained in the Declaration of Helsinki, or with the laws and regulations of the country in which the research was conducted, whichever provides greater protection of the human subjects.
Certain information about clinical trials, including a description of the study, participation criteria, location of study sites, and contact information, is required to be sent to the National Institutes of Health, (“NIH”) for inclusion in a publicly-accessible database that is available at www.clinicaltrials.gov. Sponsors also are subject to certain state laws imposing requirements to make publicly available certain information on clinical trial results. In addition, the Food and Drug Administration Amendments Act of 2007 directed the FDA to issue regulations that will require sponsors to submit to the NIH the results of all controlled clinical studies, other than Phase 1 studies.
New Drug Applications (“NDA”)
If and when the company believe that all the requisite clinical trials for a product candidate have been completed with satisfactory and supporting clinical, toxicology, safety and manufacturing-related data, the company must submit an NDA to the FDA in order to obtain approval for the marketing and sale of a product candidate in the U.S. Among many other items, an NDA typically includes the results of all preclinical and toxicology studies and human clinical trials and a description of the manufacturing process and quality control methods. The FDA must approve the NDA prior to the marketing and sale of the related product. The FDA may deny or reject an NDA if it believes all applicable regulatory criteria are not satisfied, or it may require additional data, including clinical, toxicology, safety or manufacturing data prior to approval. The FDA has 60 days from its receipt of an NDA to review the application to ensure that it is sufficiently complete for a substantive review before accepting it for filing. The FDA may request additional information rather than accept an NDA for filing. In this event, the NDA must be amended with any additional information requested. The FDA may also refer applications for novel drug products or drug products which present difficult questions of safety or efficacy to an advisory committee, typically a panel that includes clinicians and other experts, for review, evaluation and a recommendation as to whether the application should be approved. The FDA is not bound by the recommendation of an advisory committee.
An NDA can receive either standard or priority review. A product candidate representing a potentially significant improvement in the treatment, prevention or diagnosis of a life threatening or serious disease may receive a priority review. In addition, product candidates studied for their safety and effectiveness in treating serious or life-threatening illnesses that provide meaningful therapeutic benefit over existing treatments may also receive accelerated approval on the basis of adequate and well-controlled clinical trials establishing that the drug product has an effect on a surrogate endpoint that is reasonably likely to predict clinical benefit, or on the basis of an effect on a clinical endpoint other than survival or irreversible morbidity. Priority review and accelerated approval do not change the standards for approval, but may expedite the approval process.
If the results of the FDA’s evaluation of the NDA and inspection of manufacturing facilities are favorable, the FDA may issue an approval letter. An approval letter authorizes the commercial marketing of the drug with specific prescribing information for a specific indication. As a condition of NDA approval, the FDA may require post-approval testing, including Phase 4 trials, and surveillance to monitor the drug’s safety or efficacy and may impose other conditions, including labeling or distribution restrictions which can materially impact the potential market and profitability of the drug. Once granted, product approvals may be withdrawn if compliance with regulatory standards is not maintained or problems are identified following initial marketing.
If the FDA determines that it cannot approve the NDA in its present form, it generally issues what is referred to as a complete response letter. A complete response letter will describe all of the specific deficiencies that the agency has identified in an application that must be met in order to secure final approval of the NDA. If and when those conditions are met to the FDA’s satisfaction, the FDA will typically re-review the application and possibly issue an approval letter. However, even after submitting this additional information, the FDA ultimately may decide that the application does not satisfy the regulatory criteria for approval. It can take several years for the FDA to approve a NDA once it is submitted, and the actual time required for any product candidate to be approved may vary substantially, depending upon the nature, complexity and novelty of the product candidate.
The company cannot assure you that the FDA, or any other similar regulatory authority in another country, will grant approval for any of its product candidates on a timely basis, if at all. Success in preclinical or early-stage clinical trials does not assure success in later stage clinical trials. Data obtained from preclinical and clinical activities is not always conclusive and may be susceptible to varying interpretations that could delay, limit or prevent regulatory approval.
Post-Approval Regulations
If and when a product candidate receives regulatory approval to be marketed and sold, the approval is typically limited to a specific clinical indication or use. Further, even after regulatory approval is obtained, subsequent discovery of previously unknown safety problems with a product may result in restrictions on its use, or even complete withdrawal of the product from the market. Any FDA-approved products manufactured or distributed by it are subject to continuing regulation by the FDA, including record-keeping requirements and reporting of adverse events or experiences. Further, drug manufacturers and their subcontractors are required to register their establishments with the FDA and state agencies, and are subject to periodic inspections by the FDA and state agencies for compliance with cGMP regulations, which impose rigorous procedural and documentation requirements upon it and its contract manufacturers. The company cannot be certain that we, or its present or future contract manufacturers or suppliers, will be able to comply with cGMP regulations and other FDA regulatory requirements. Failure to comply with these requirements may result in, among other things, total or partial suspension of production activities for its current and future product candidates, failure of the FDA to grant approval for the marketing of such product candidates, and withdrawal, suspension, or revocation of marketing approvals.
If the FDA approves one or more of its product candidates, the company and its contract manufacturers must provide the FDA with certain updated safety, efficacy and manufacturing information. Product changes, as well as certain changes in the manufacturing process or facilities where the manufacturing occurs or other post-approval changes may necessitate additional FDA review and approval. The company rely, and expect to continue to rely, on third parties for the formulation and manufacture of clinical and commercial quantities of its products. Future FDA and state inspections may identify compliance issues at the facilities of its contract manufacturers that may disrupt production or distribution, or require substantial resources to correct.
The labeling, advertising, promotion, marketing and distribution of an approved drug or biologic product must also comply with FDA and Federal Trade Commission, (“FTC”) requirements which include, among others, standards and regulations for direct-to-consumer advertising, off-label promotion, industry sponsored scientific and educational activities, and promotional activities involving the Internet. The FDA and FTC have very broad enforcement authority, and failure to abide by these regulations can result in penalties, including the issuance of a warning letter directing the company to correct deviations from regulatory standards and enforcement actions that can include seizures, fines, injunctions and criminal prosecution.
Once an approval is granted, the FDA may withdraw the approval if compliance with regulatory standards is not maintained or if problems occur after the product reaches the market. After approval, some types of changes to the approved product, such as adding new indications, manufacturing changes and additional labeling claims, are subject to further FDA review and approval. In addition, the FDA may require testing and surveillance programs to monitor the effect of approved products that have been commercialized, and in some circumstances the FDA has the power to prevent or limit further marketing of a product based on the results of these post-marketing programs.
From time to time, legislation is drafted and later introduced and passed that could significantly change the statutory provisions governing the approval, manufacturing and marketing of products regulated by the FDA. In addition, FDA regulations and guidance are often revised or reinterpreted by the agency in ways that may significantly affect its business and its product candidates. It is impossible to predict whether legislative changes will be enacted, or whether FDA regulations, guidance or interpretations will change or what the impact of such changes, if any, may be. The company cannot predict the likelihood, nature or extent of adverse governmental regulation that might arise from future legislative or administrative action, either in the U.S. or abroad, or the impact such changes could have on its business.
Other U.S. Health Care Laws and Compliance Requirements
In the U.S., its activities are subject to regulation by various federal, state and local authorities in addition to the FDA, including the Centers for Medicare and Medicaid Services (formerly the Health Care Financing Administration), other divisions of HHS (e.g., the Office of Inspector General), the U.S. Department of Justice and individual U.S. Attorney offices within the Department of Justice, and state and local governments. For example, sales, marketing and scientific/educational grant programs must comply with the anti-fraud and abuse provisions of the Social Security Act, the False Claims Act, the privacy provisions of the Health Insurance Portability and Accountability Act (“HIPAA”) and similar state laws, each as amended. Pricing and rebate programs must comply with the Medicaid rebate requirements of the Omnibus Budget Reconciliation Act of 1990 and the Veterans Health Care Act of 1992, each as amended. If products are made available to authorized users of the Federal Supply Schedule of the General Services Administration, additional laws and requirements apply. Under the Veterans Health Care Act, (“VHCA”), drug companies are required to offer certain drugs at a reduced price to a number of federal agencies including the U.S. Department of Veterans Affairs and U.S. Department of Defense, the Public Health Service and certain private Public Health Service designated entities in order to participate in other federal funding programs including Medicare and Medicaid. Recent legislative changes purport to require that discounted prices be offered for certain U.S. Department of Defense purchases for its TRICARE program via a rebate system. Participation under VHCA requires submission of pricing data and calculation of discounts and rebates pursuant to complex statutory formulas, as well as the entry into government procurement contracts governed by the Federal Acquisition Regulations.
In March 2010, the ACA was signed into law, which intended to broaden access to health insurance, reduce or constrain the growth of healthcare spending, enhance remedies against fraud and abuse, add transparency requirements for the healthcare and health insurance industries, impose taxes and fees on the health industry and impose additional health policy reforms. Implementation of the ACA has substantially changed healthcare financing and delivery by both governmental and private insurers, and significantly impacted the pharmaceutical industry. The ACA, among other things, established an annual, nondeductible fee on any entity that manufactures or imports certain specified branded prescription drugs and biologic agents, revised the methodology by which rebates owed by manufacturers to the state and federal government for covered outpatient drugs under the Medicaid Drug Rebate Program are calculated, increased the minimum Medicaid rebates owed by most manufacturers under the Medicaid Drug Rebate Program, extended the Medicaid Drug Rebate program to utilization of prescriptions of individuals enrolled in Medicaid managed care organizations, and provided incentives to programs that increase the federal government's comparative effectiveness research. Since its enactment there have been judicial and Congressional challenges to certain aspects of the ACA, and the company expect there will be additional challenges and amendments to the ACA in the future. There is currently uncertainty with respect to the impact any such challenges and amendments may have and any resulting changes may take time to unfold, which could have an impact on coverage and reimbursement for healthcare items and services covered by plans that were authorized by the ACA.
In order to distribute products commercially, the company must comply with state laws that require the registration of manufacturers and wholesale distributors of pharmaceutical products in a state, including, in certain states, manufacturers and distributors who ship products into the state even if such manufacturers or distributors have no place of business within the state. Some states also impose requirements on manufacturers and distributors to establish the pedigree of product in the chain of distribution, including some states that require manufacturers and others to adopt new technology capable of tracking and tracing a product as it moves through the distribution chain. Several states have enacted legislation requiring pharmaceutical companies to establish marketing compliance programs, file periodic reports with the state, make periodic public disclosures on sales, marketing, pricing, clinical trials and other activities or register their sales representatives, as well as prohibiting pharmacies and other health care entities from providing certain physician prescribing data to pharmaceutical companies for use in sales and marketing, and prohibiting certain other sales and marketing practices. All of its activities are potentially subject to federal and state consumer protection and unfair competition laws.
Foreign Regulation
In addition to regulations in the U.S., Aviragen Therapeutics is subject to a variety of foreign regulations governing clinical trials and commercial sales and distribution of its product candidates to the extent the company choose to develop these product candidates or sell any products outside of the U.S. Whether or not the company obtain FDA approval for a product, the company must obtain similar approval by comparable regulatory authorities in foreign countries before the company can commence clinical trials or the marketing of a product in those countries. The approval process varies from country to country and the time may be longer or shorter than that required to obtain FDA approval. The requirements governing the conduct of clinical trials, product licensing, pricing and reimbursement vary greatly from country to country.
European Union (“EU”) member states require both regulatory clearances by the national competent authority and a favorable ethics committee opinion prior to the commencement of a clinical trial. Under the EU regulatory systems, the company may submit marketing authorization applications either under a centralized or decentralized procedure. The centralized procedure provides for the grant of a single marketing authorization that is valid for all EU member states. The centralized procedure is compulsory for medicines produced by certain biotechnological processes, products with a new active substance indicated for the treatment of certain diseases and products designated as orphan medicinal products and optional for those products which are highly innovative or for which a centralized process is in the interest of patients. The decentralized procedure of approval provides for approval by one or more other, or concerned, member states of an assessment of an application performed by one member state, known as the reference member state. Under the decentralized approval procedure, an applicant submits an application, or dossier, and related materials (draft summary of product characteristics, draft labeling and package leaflet) to the reference member state and concerned member states. The reference member state prepares a draft assessment and drafts of the related materials within 120 days after receipt of a valid application. Within 90 days of receiving the reference member state’s assessment report, each concerned member state must decide whether to approve the assessment report and related materials. If a member state cannot approve the assessment report and related materials on the grounds of potential serious risk to public health, the disputed points may eventually be referred to the European Commission, whose decision is binding on all member states.
Pharmaceutical Coverage, Pricing and Reimbursement
Significant uncertainty exists as to the coverage and reimbursement status of any pharmaceutical products for which the company may obtain regulatory approval to market and sell. In the U.S. and other countries, revenue from any products for which the company receive regulatory approval to sell will depend considerably on the availability of reimbursement from third-party payers. Third-party payers include government health administrative authorities, managed care providers, private health insurers and other organizations. The process for determining whether a payer will provide coverage for a product may be separate from the process for setting the price or reimbursement rate that the payer will pay for the product. Third-party payers may limit coverage to specific products on an approved list, or formulary, which might not include all of the FDA-approved products for a particular indication. Third-party payers are increasingly challenging the price and examining the medical necessity and cost-effectiveness of medical products and services, in addition to their safety and efficacy. The company may need to conduct expensive pharmacoeconomic studies in order to demonstrate the medical necessity and cost-effectiveness of its products, which would be in addition to the costs required to obtain FDA approvals. Its products may not be considered medically necessary or cost-effective. A payer’s decision to provide coverage for a product does not imply that an adequate reimbursement rate will be approved. Adequate third-party reimbursement may not be available to enable it to maintain price levels sufficient to realize an appropriate return on its investment in developing a product.
In 2003, the U.S. government enacted legislation providing a prescription drug benefit for Medicare recipients, which became effective at the beginning of 2006. Government payment for some of the costs of prescription drugs may increase demand for any products for which the company receive marketing approval. However, to obtain payments under this program, the company would be required to sell products to Medicare recipients through prescription drug plans operating pursuant to this legislation. These plans will likely negotiate discounted prices for its products. In March 2010, the Patient Protection and Affordable Care Act became law in the U.S., which substantially changed the way healthcare is financed by both governmental and private insurers. The company anticipate that this legislation will result in additional downward pressure on the price, if any, that the company may receive for any approved product. Federal, state and local governments in the U.S. continue to consider legislation to limit the growth of health care costs, including the cost of prescription drugs. Future legislation could limit payments for pharmaceutical products, including the product candidates that Aviragen Therapeutics is developing.
Different pricing and reimbursement schemes exist in other countries. In the EU, governments influence the price of pharmaceutical products through their pricing and reimbursement rules and control of national health care systems that fund a large part of the cost of those products to consumers. Some jurisdictions operate positive and negative list systems under which products may only be marketed once a reimbursement price has been agreed. To obtain reimbursement or pricing approval, some of these countries may require the completion of clinical trials that compare the cost-effectiveness of its particular drug products to currently available therapies. Other member states allow companies to fix their own prices for medicines, but monitor and control company profits. The downward pressure on health care costs in general, particularly prescription drugs, has become very intense. As a result, increasingly high barriers are being erected to the entry of new products. In addition, in some countries, cross-border imports from low-priced markets exert a commercial pressure on pricing within a country.
The marketability of any products for which the company receive regulatory approval to sell may suffer if the government and third-party payers fail to provide adequate coverage and reimbursement. In addition, an increasing emphasis on managed care in the U.S. has increased, and the company expect will continue to increase the pressure on pharmaceutical pricing. Coverage policies and third-party reimbursement rates may change at any time. Even if favorable coverage and reimbursement status is attained for one or more products for which the company receive regulatory approval, less favorable coverage policies and reimbursement rates may be implemented in the future.
Employees
As of June 30, 2017, the company had 16 full-time employees, seven of whom were engaged in research and development, and nine of whom were engaged in corporate, administration, finance, and business development activities. All of its employees have entered into non-disclosure agreements with it regarding its intellectual property, trade secrets and other confidential information. None of its employees are represented by a labor union or covered by a collective bargaining agreement, nor have the company experienced any work stoppages. The company believe that the company maintain satisfactory relations with its employees.




